DYNAMIC CHANGES IN BLOOD PARAMETERS OF
LIVER TRANSPLANTATION RECIPIENTS
PRE AND POST COVID-19 INFECTION
LIVER TRANSPLANTATION RECIPIENTS
PRE AND POST COVID-19 INFECTION
Abstract
The effect of liver transplantation (LT) on the severity and mortality of coronavirus disease 2019 (COVID-19) remained controversial. There is still no consensus on whether liver transplantation (LT) recipients with COVID-19 are at greater risk of developing severe or fatal COVID-19. It is not completely clear what is the course of the disease and what laboratory changes occur. The present study was undertaken to identify the dynamic changes in blood parameters of LT recipients pre and post COVID-19 infection which may be used to diagnose the severity and thus assess the prognosis of such patients. Our collected data are from a Bulgarian liver transplantation program at a single center for adult recipients of LT who were followed up from May, 2020, through May, 2022 in the pandemic environment. The current study aims analyzing the statistically significant differences in over 50 biochemical blood parameters in the cohort of LT recipients pre and post SARS-CoV-2 infection.Citation details of the article
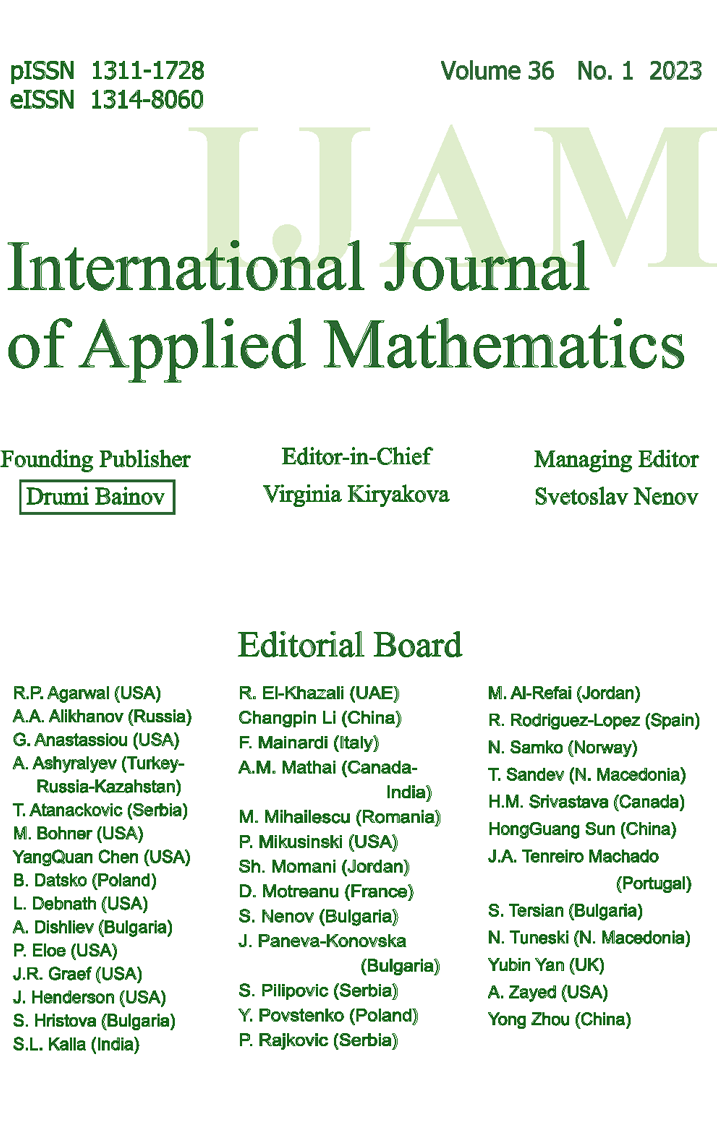
Journal: International Journal of Applied Mathematics Journal ISSN (Print): ISSN 1311-1728
Journal ISSN (Electronic): ISSN 1314-8060
Volume: 35 Issue: 4 Year: 2022 DOI: 10.12732/ijam.v35i4.10
Download Section
Download the full text of article from here.
You will need Adobe Acrobat reader. For more information and free download of the reader, please follow this link.
References
- [1] G. Snedecor, W. Cochran, Statistical Methods, Iowa State University Press, Iowa (1989).
- [2] E. Hincal, B. Kaymakamzade, N. Gokbulut, Humidity level on Covid-19 with control strategies, International Journal of Applied Mathematics, 34, No 4 (2021), 795-802; doi:10.12732/ijam.v34i4.14.
- [3] StatSoft, Inc., STATISTICA Manual (Data Analysis Software System), Version 13.0 (2019).
- [4] C. Ronco, T. Reis, Kidney involvement in COVID-19 and rationale for extracorporeal therapies, Nat. Rev. Nephrol, 16, No 6 (2020), 308-310; doi: 10.1038/s41581-020-0284-7.
- [5] A. Romanelli, S. Mascolo, Immunosuppression drug-related and clinical manifestation of coronavirus disease 2019: a therapeutical hypothesis, Amer. J. Transplan., 20, No 7 (2020), 1947-1948; doi: 10.1111/ajt.15905.
- [6] V. Terzieva, Y. Uzunova, R. Gornev, L. Spassov, Regulatory T cells in the mosaic of liver transplantation tolerance, In: V. Mihaylov (Ed.), Organ Donation and Transplantation, London (2020); https://www.intechopen.com/chapters/73970; doi: 10.5772/intechopen.94362.
- [7] S. Thompson, M. K. Bohn, N. Mancini, et al., Horvath and the IFCC taskforce on COVID 19. IFCC interim guidelines on biochemical/hematological monitoring of COVID 19 patients, Clin. Chem. Lab. Med., 58, No 12 (2020), 2009-2016; doi: 10.1515/cclm-2020-1414.
- [8] L. Zhang, Y. Peng, Q. Zheng, L. Jiang, S. Tang, P. Chen, Retrospective analysis of clinical characteristics and laboratory results of COVID 19 patients, European J. of Inflammation, 19 (2021), 1-7; doi:10.1177/20587392211011919.
- [9] S. Ghahramani, R. Tabrizi, K.B. Lankarani, S. M. Kashani, S. Rezaei, N. Zeidi, M. Akbari, S.T. Heydari, H. Akbari, P. Nowrouzi-Sohrabi, F. Ahmadizar, Laboratory features of severe vs. Non-severe COVID 19 patients in Asian populations: A systematic review and meta analysis, Eur. J. Med. Res., 25, Art. No 30 (2020), 1-10; https://doi.org/10.1186/s40001020-00432-3.632 N.N. Yurukova
- [10] C. Danwang, F.T. Endomba, J.R. Nkeck, D.L.A. Wouna, A. Robert, J.J. Noubiap, A meta-analysis of potential biomarkers associated with severity of coronavirus disease 2019 (COVID 19), Biomark. Res. 8, Art. No 37 (2020), 1-13; https://doi.org/10.1186/s40364-020-00217-0.
- [11] L. Lazarova, N. Stoikovikj, A. Stojanova, M. Mileva, M. Ljubenovska, Mathematical model for prediction of Covid-19 dynamics, International Journal of Applied Mathematics, 35, No 1 (2022), 119-133; doi:10.12732/ijam.v35i1.9.